By Emily Ayshford
By diving deep into the gut’s delicate community of bacteria, viruses, fungi and microbes, UChicago experts unlock lifesaving insights and new treatments.
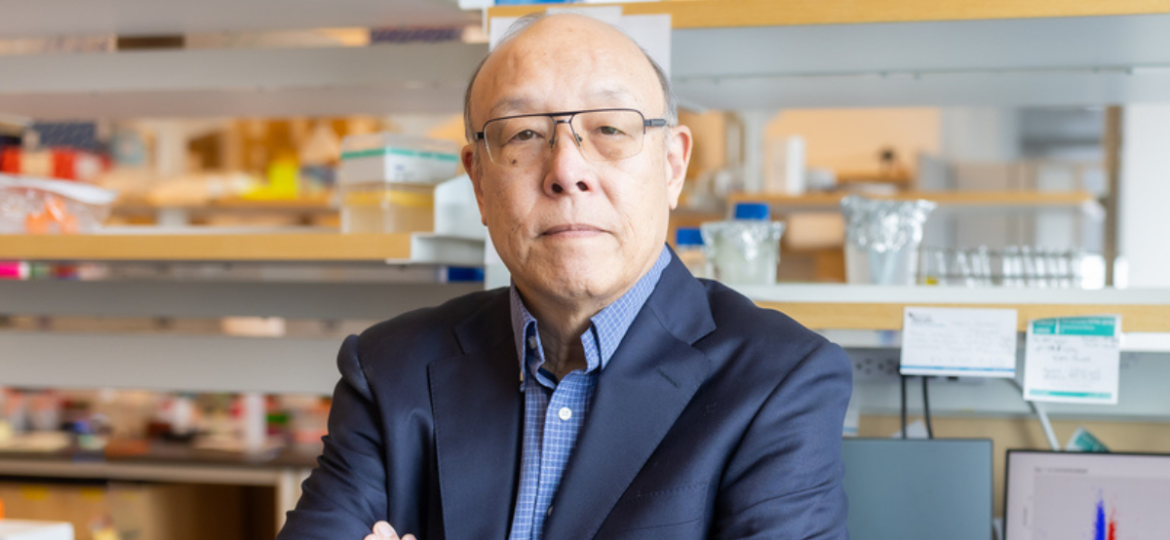
Nearly a quarter-century ago, Eugene Chang, MD’76, was studying inflammatory bowel diseases, chronic yet poorly understood conditions marked by diarrhea, pain and fatigue — sometimes with life-threatening complications.
Cases of IBD had been rising for decades, but researchers at the time couldn’t determine why. The cause wasn’t just genetics, environmental factors or even one triggering pathogen. Chang suspected part of the answer could lie within our own gut microbiome — an ever-changing network of trillions of microbes that has co-evolved over time to help the body digest food.
Clearly, these bacteria were doing far more than just digesting. “It dawned on us that the gut microbes were affecting our gene expression,” said Chang, Martin Boyer Professor of Medicine at the University of Chicago.
The hunch was so strong that Chang retooled his namesake lab in 2000 to focus on the microbiome, collaborating with scientists at Argonne National Laboratory and the Marine Biological Laboratory, and using the latest technologies to study microbes in detail.
Some colleagues questioned the pivot. “There was so little known about the microbiome, and most people were very skeptical that it could be studied,” Chang said. “You’re dealing with trillions of microbes. How do you sort that out?”
Today, the pursuit is booming at the University of Chicago. The gut microbiome has been implicated in a host of diseases and conditions, including those that affect the gastrointestinal tract. It has also been linked to metabolic diseases like diabetes and obesity, cancers, complex immune diseases, allergies, developmental abnormalities and neurological disorders.
As researchers untangle the web of microbiome and host, University teams are developing new breakthroughs that include management tools for IBD, metabolites to treat allergies and probiotics to improve liver disease outcomes.
Read the full story in Medicine on the Midway.